
Blue Light
Treatment for Skin Lesions
Blue Light as a treatment for skin lesions
Emoled studies the effects of blue LED light in the treatment of skin lesions in collaboration with some of the leading Italian research centres in physics and medicine.
A broad range of diseases is studied, including chronic skin lesions such as ulcers of the lower limbs (venous, arterial and mixed ulcers), inflammatory ulcers (from rheumatic diseases, scleroderma), diabetic foot and pressure ulcers, skin lesions with massive tissue loss such as burns and trauma wounds, surgical wound dehiscence, and dermatological disorders.
This research has led to the discovery that blue light is able to resolve inflammation and stimulate skin tissue regeneration via the process of photobiomodulation.
Origins
While sunlight has been used since ancient times to treat certain diseases, modern phototherapy came about following the work of the Danish dermatologist Finsen who was awarded the Nobel Prize in Medicine in 1903, following the publication of the results of lupus vulgaris treatment with concentrated and UV-rich light generated by an arc lamp.
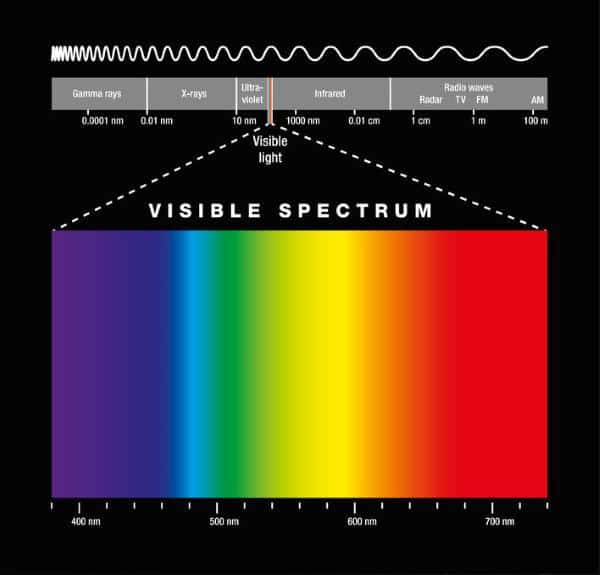
Following the development of lasers in the 60s and then LEDs (Light Emitting Diodes), light sources that emit “monochromatic” light, it has been possible to investigate the interaction between biological tissues and specific wavelengths. This was the birth of Biophotonics, the branch of physics studying such interactions, and that has led to the development of various medical devices for therapeutic and diagnostic treatments.

The therapeutic mechanism of blue light:
Photobiomodulation.
The therapeutic effect of light occurs thanks to the presence of endogenous molecules in an organism’s tissues that are capable of absorbing light. The energy conveyed by the light spectrum is absorbed by these naturally existing elements, known as “chromophores”, and is used to promote chemical reactions or produce conformational changes in certain biomolecules.
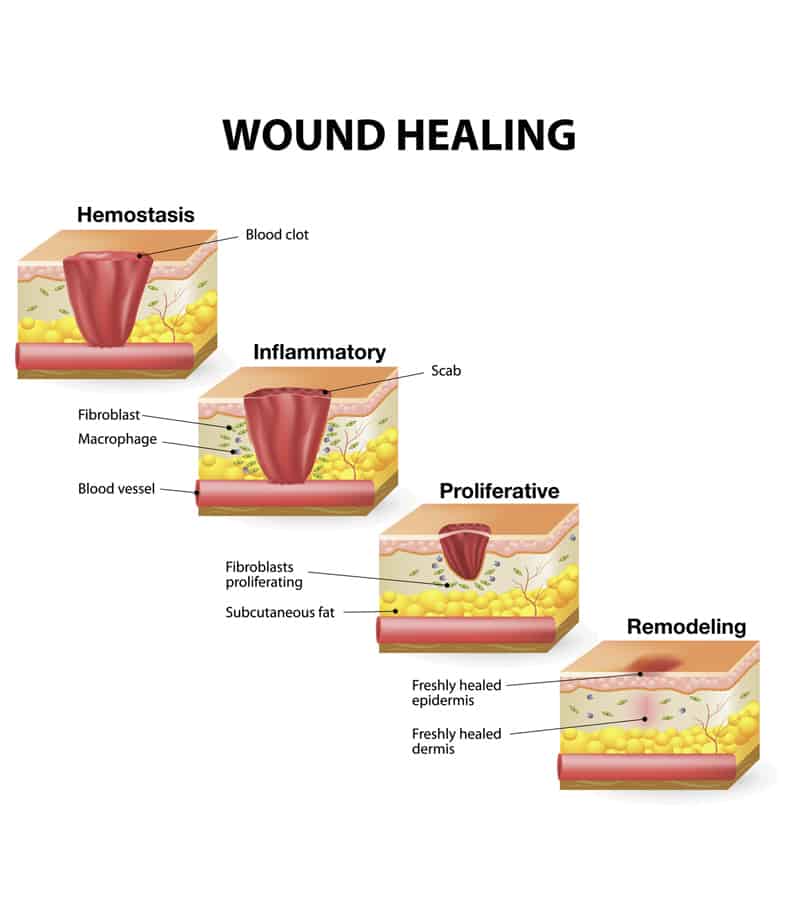
This process translates into beneficial therapeutic effects such as reduction of pain and inflammation. The immunomodulation and induction of wound healing and tissue regeneration was defined as “Photobiomodulation” in 2014 by the North American Association for Laser Therapy and by the World Association for Laser Therapy at a joint conference.
Each chromophore has a different absorption spectrum and therefore a different sensitivity to various wavelengths which, once absorbed by tissues, can produce varying photophysical and photochemical effects.
Emoled has developed a photobiomodulation-based therapy for skin lesions that uses specific wavelengths of visible light spectrum in the blue range. Blue light is absorbed by electron transport chain enzymes and by flavoproteins.
Its therapeutic effects include resolving inflammation, reducing pain and stimulating tissue regeneration, as observed in preclinical and clinical studies.
A therapy for hard-to-heal wounds,
a major health problem
Inflammation is a necessary phase in the wound repair process that should last no more than four weeks in total. Due to diseases or specific physical conditions (such as old age, nutritional deficits and mobility restrictions), the inflammatory phase can stall, causing the wound to become chronic. The most widespread and impacting aetiologies of chronic wounds are lower leg ulcers, deriving predominantly from venous insufficiency; these affect 1% of the adult population and 3.6% of the population over age 65. Diabetic foot, which affects one diabetes mellitus patient out of three is the most frequent cause of lower limb amputation in the world. Pressure or “decubitus” ulcers caused by the pressure of a bone prominence in people with limited mobility, such as patients in intensive care, have an average prevalence of 13.7% in the European population.
A poorly regulated inflammatory response can also give rise to complications in wounds with major tissue loss, caused by a trauma or a burn, and to surgical wound dehiscence.
Photobiomodulation with blue light, a therapy that can stimulate inflammatory phase transition, can contribute to the resolution of wounds with a delayed or not-completed healing process. Such wounds represent a major healthcare problem given the high costs of management and the low quality of life of patients affected by them.
Action on fibroblasts and scarring outcomes
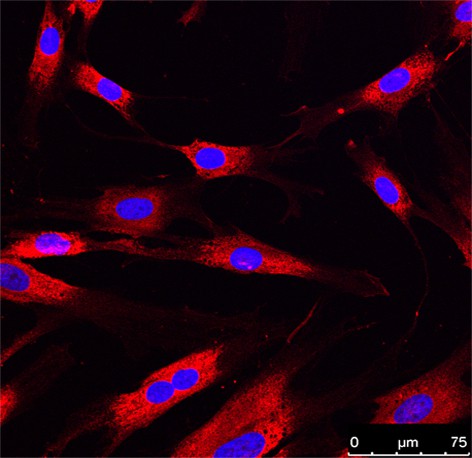
Fibroblasts are the most numerous cells in the connective tissue of the skin and play a fundamental role in its reconstruction following damage. Preclinical studies have demonstrated that blue light can modulate the activity of fibroblasts. The metabolism and proliferation of these cells are increased or, alternatively, inhibited, depending on the dose of light used for irradiating them.
In addition, better outcomes in terms of organisation and morphology of collagen in wounds treated with blue light have been found compared to control. Based on this evidence, photobiomodulation with blue light can contribute to a good scarring outcome and could be used in the treatment and prevention of keloids, abnormal scar tissue that can develop following abrasions and wounds, where the cause lies in the hyperactivity of fibroblasts.
References:
Anders JJ et al. Low-Level Light/Laser Therapy Versus Photobiomodulation Therapy. Photomedicine and Laser Surgery Volume 33, Number 4, 2015 Pp. 183–184; DOI: 10.1089/pho.2015.9848.
Cicchi R et al. Observation of an improved healing process in superficial skin wounds after irradiation with a blue-LED haemostatic device J. Biophotonics 9, No. 6, 645–655 (2016); doi:10.1002/jbio.201500191.
Dini V et al. Blue light emission in the management of hard-to-heal wounds. Italian Journal of Dermatology and Venerology, 2020;155; doi: 10.23736/S0392-0488.20.06691-2.
Fraccalvieri M et al. Effectiveness of Blue light photobiomodulation therapy in the treatment of chronic wounds. Results of the Blue Light for Ulcer Reduction (B.L.U.R.) Study. Italian Journal of Dermatology and Venerology, 2021, Sep 09. DOI: 10.23736/S2784-8671.21.07067-5.
Han G, Ceilley R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv Ther. 2017;34(3):599-610. doi:10.1007/s12325-017-0478-y.
Nair HK, Bin Sulong MAA. Effects of photobiomodulation with blue light on diabetic foot ulcers: a case series report. Wounds Asia. 2021, Vol 4 Issue 3, pag. 42-47.
Magni G et al. Blue LED light modulates inflammatory infiltrate and improves the healing of superficial wounds. Photodermatol Photoimmunol Photomed 2019;00:1–3; doi:10.1111/phpp.12527.
Magni M et al. Experimental Study on Blue Light Interaction with Human Keloid-Derived Fibroblasts Biomedicines 2020, 8, 573; doi:10.3390/biomedicines8120573.
Marchelli M et al. Photobiomodulation with Blue Light in non-healing wounds: case series evaluation. Wounds International 2019, Volume 10 Issue 3, pag 63-67.
Moore Z et al. The prevalence of pressure ulcers in Europe, what does the European data tell us: a systematic review. Journal of Wound Care Vol 28, No 11, November 2019.
Orlandi C et al. Blue Led Light in Burns: A New Treatment’s Modality. J Clin Investigat Dermatol. 2021, 9(2):5.
Rastogi A et al. Long term outcomes after incident diabetic foot ulcer: Multicenter large cohort prospective study (EDI-FOCUS investigators) epidemiology of diabetic foot complications study: Epidemiology of diabetic foot complications study. Diabetes Res Clin Pract. 2020 Apr;162:108113.
Ricci E, Pittarello M. Blue light photobiomodulation for reactivation of healing in wounds not responding to standard therapy. J Wound Care. 2023 Nov 2;32(11):695-703. doi:10.12968/jowc.2023.32.11.695. PMID: 37907354.
Rossi F at al. Photobiomodulation of Human Fibroblasts and Keratinocytes with Blue Light: Implications in Wound Healing Biomedicines 2021, 9, 41; doi.org/10.3390/biomedicines9010041.
Shubhangi VA. Chronic Leg Ulcers: Epidemiology, Aetiopathogenesis, and Management. Ulcers, Volume 2013, Article ID 413604, 9 pages http://dx.doi.org/10.1155/2013/413604
Spinella A et al. Photobiomodulation Therapy: A New Light in the Treatment of Systemic Sclerosis Skin Ulcers. Rheumatol Ther. 2022 Jun;9(3):891-905. doi: 10.1007/s40744-022-00438-9. Epub 2022 Mar 25. PMID: 35334095; PMCID: PMC9127012.
Zhang Y et al. Global Disability Burdens of Diabetes-Related Lower-Extremity Complications in 1990 and 2016. Diabetes Care. 2020 May;43(5):964-974.
