
Study on the reactivation of wound healing with Blue Light
Title: Blue light photobiomodulation for reactivation of healing in wounds not responding to standard therapy
Authors: Ricci E, Pittarello M
Year: 2023
Publication: J Wound Care. 2023 Nov 2;32(11):695-703. DOI: 10.12968/jowc.2023.32.11.695
SUMMARY
A single-center observational study that had the aim of evaluating the efficacy of Photobiomodulation with blue light (EmoLED) in activating the healing process of wounds not responsive to standard treatment. Patients with lower limb skin lesions that were not responsive to standard treatment were enrolled. Wounds that did not heal sufficiently in 4 weeks (i.e. at least 40% reduction in wound area) were considered as non-responsive to therapy (run-in period). Following enrollment, Blue Light was applied to patients on a weekly basis for 4 weeks to determine its efficacy in activating the healing process; the entire wound area was irradiated for 120 seconds. Patients were then observed for another 4-week period. The run-in period was intended to provide a comparator. The parameters used to evaluate wounds were reduction in area (cm2), change in wound bed score (WBS), change in pain measured with Numerical Rating Scale (NRS), and complete healing (100% reduction in wound area). The parameters were analysed by comparing the values at t0 (= start of observation) with the values at t28 (=start of the 4-week Blue Light treatment), t56 (=start of the 4-week observation period after Blue Light treatment), t84 (=end of the 4-week observation period after Blue Light treatment). The analysis was also conducted by wound aetiology and duration.
Results
The study enrolled 60 patients, of whom one patient dropped out; and thus a total of 59 patients were evaluated. The mean age of the cohort was 70.6 years and 66.1% were female. The mean duration of the wound was 23.9 months. Wounds were put into subgroups according to aetiology:
- Hard-to-heal venous wounds (30.5%)
- Hard-to-heal arterial and mixed wounds (16.9%)
- Hard-to-heal inflammatory wounds (e.g., vasculitis, connective tissue disease and Martorell’s ulcer, 22.0%)
- Other hard-to-heal wounds (e.g., pyoderma and osteomyelitis 13.6%)
- Acute wounds (16.9%).
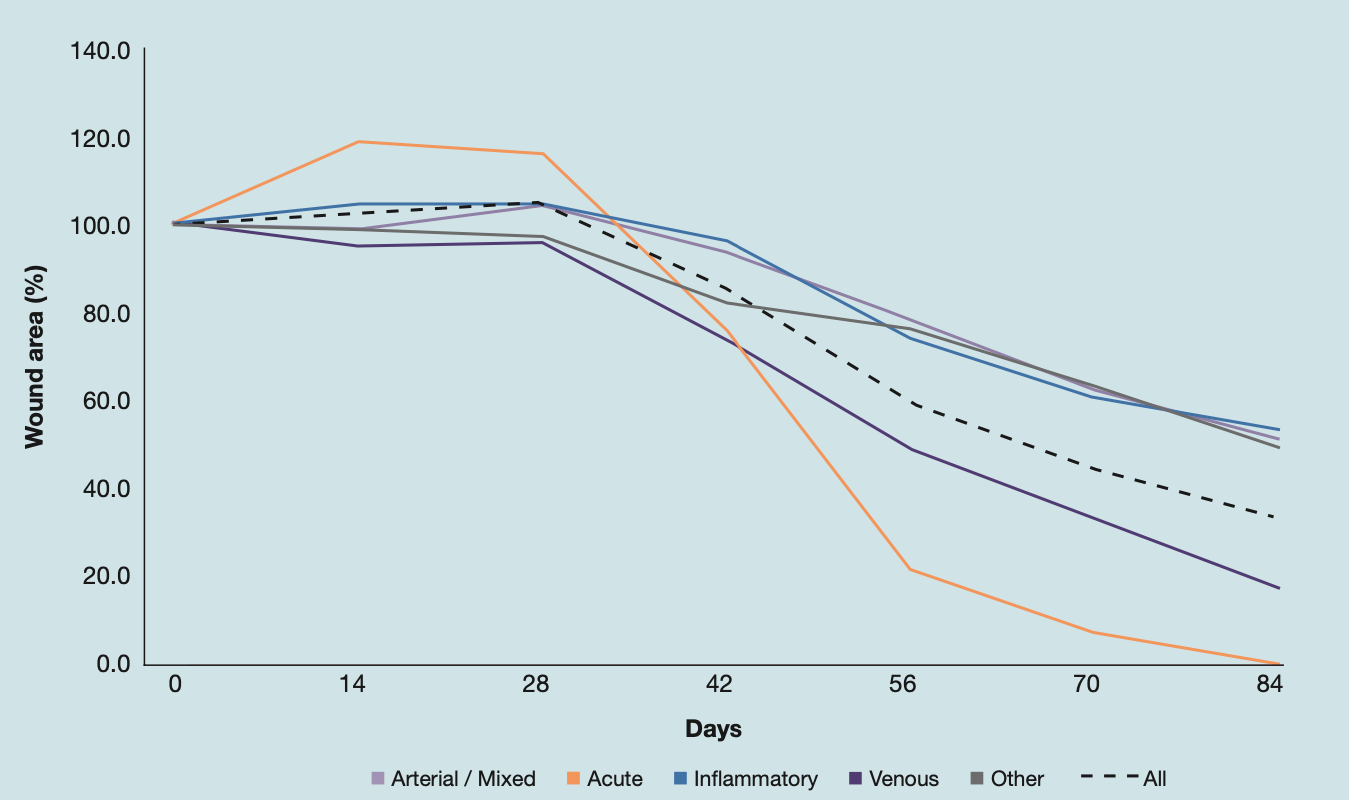
Wound area. In the run-in period the wound area showed no appreciable improvement, while following photobiomodulation there was a marked decrease in all subgroups. The mean reduction in wound area at the end of the blue light treatment period (t56) compared to baseline (t0) was 51.38% (p <0.001) for all wounds. Among subgroups, the best performance was obtained for chronic venous wounds, achieving a 63.36% (p <0.001) mean reduction, and acute wounds, achieving a mean reduction of 82.76% (p <0.001). The reduction in mean area obtained at the end of the post-treatment observation period (t84) compared to baseline (t0) was 76.10% (p <0.001) for all wounds, 94% for chronic venous wounds, while all acute wounds achieved complete healing (100% mean wound are reduction, p <0.001). There was no significant difference between subgroups by wound’s age.
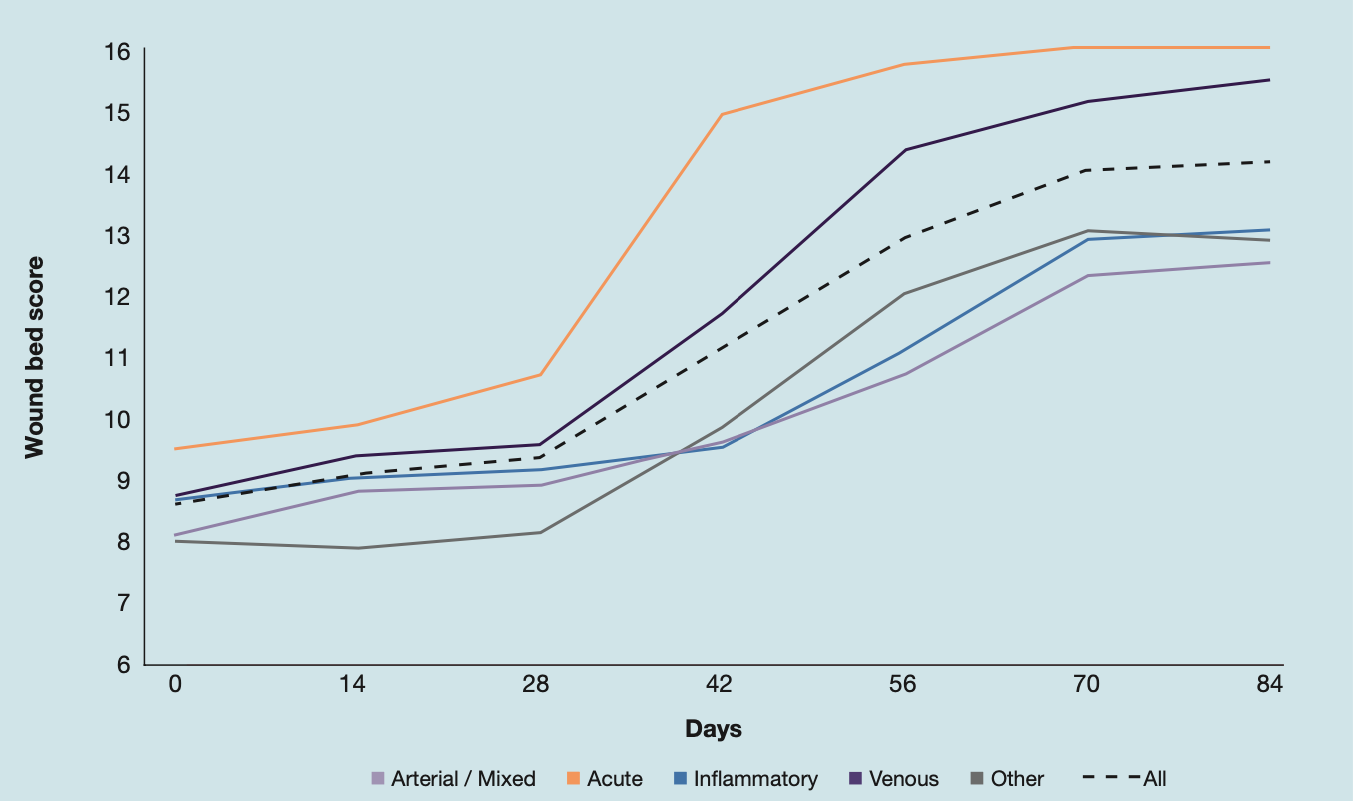
Wound bed score. The greatest mean change in WBS was seen at the end of the 4-week treatment period (t56) with blue light with an increase in the average WBS from 8.6 at t0 to 12.8 at t56 (77.2%, p <0.001). The positive trend was also maintained during the 4-week observation period after blue light treatment: at t84 a further increase in the average WBS to 14 (102.2% compared to baseline, p <0.001) was observed. Acute lesions responded best to treatment, while among chronic lesions venous ulcers showed the best response. The best results in WBS were also obtained in lesions with a duration between 6 and 12 months and >12 months.
Pain (NRS) score. There was a clear decrease in pain during blue light treatment, achieving a reduction in the average NRS from 4.3 at t0 to 1.8 at t56 (53.23%, p <0.001). After an additional 4 weeks, a further reduction to 1.0 (76.26% compared to baseline, p <0.001) in NRS pain was recorded. By wound etiology, greater improvement was seen in acute wounds (87.50%; p <.001) and venous wounds (87.96%; p <0.001), but also in inflammatory wounds (72.80%; p <0.001). Regarding wound duration, the best results were seen in wounds with a duration between 6 and 12 months, followed by wounds with ≤ 6 months duration
Complete healing. In the entire cohort, at the end of the 4-week treatment period (t56) 14 patients (23.7%) showed complete healing, which increased to 36 patients (61%) at the end of the observation period (t84). At t56, the highest proportion of complete healing was seen in patients with acute wounds (100%) and in the group with venous wounds (83.3%). Regarding wound duration, the highest percentage of healings occurred in the group of chronic wounds with shorter duration (69.2%).
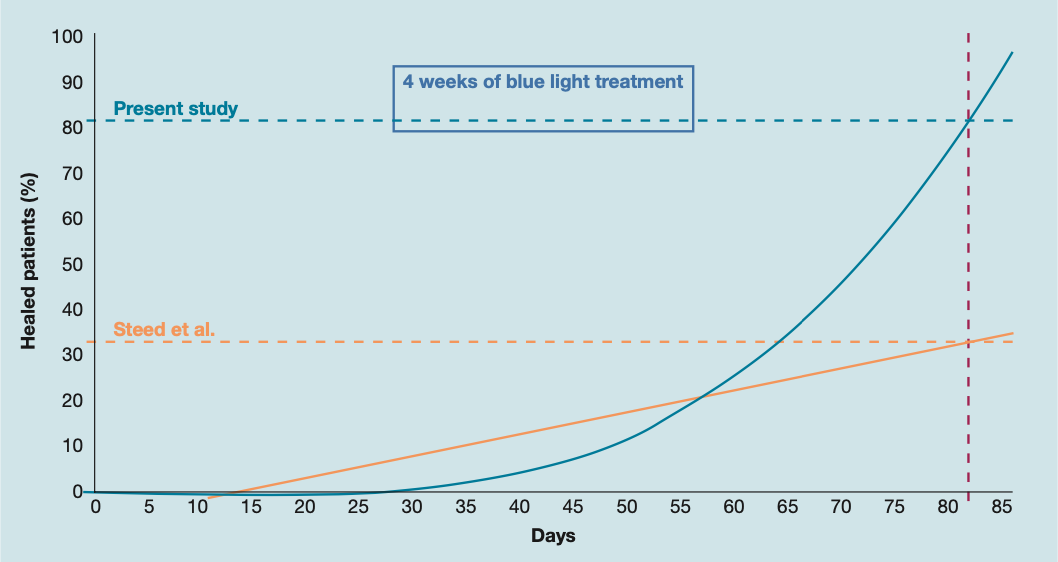
Wound healing trajectories. Wound healing trajectories are plots of percentage of wound closure versus time of wound treatment in a given patient cohort and they are discussed in the literature as an outcome measure to evaluate the efficacy of new treatments. Steed et al. (Steed DL, Hill DP, Woodske ME et al. Wound-healing trajectories as outcome measures of venous stasis ulcer treatment. Int Wound J. 2006;3(1):40-7.) previously constructed healing trajectories of patients (232) with venous leg ulcers who achieved healing within 20 weeks of SoC treatment. The trajectory of Steed et al. was compared with the healing trajectory of patients with venous leg ulcers of the study (19) built on Steed’s model, taking the study period (12 weeks = 84 days) as the reference period. At the end of the 84-day observation period, the percentage of healed lesions in Steed’s model is 32.81% compared to 81.34% in the study model. Observing the trend of the trajectories, it can be seen that the shift in the trajectory of the study patient cohort towards the trajectory of the Steed patient cohort starts on day 28, corresponding to the start of treatment with Blue Light. Furthermore, the percentage of healings observed in the study patient cohort exceeds that observed in Steed patients around day 56, which corresponds to the end of the 4 weeks of Blue Light treatment.
Discussion and conclusions
In the BLUR study, patients with venous leg ulcers treated with standard of care and blue light for 60 seconds once a week for 10 weeks achieved a mean wound area reduction of 66.7%, which is somewhat lower than 88.29% (t28-t84) observed herein; in the study by Dini et al. the subgroup of patients with hard-to-heal venous leg ulcers treated with standard of care plus blue light for 60 sec once a week for 4 weeks, achieved a mean area reduction of 36.1%, compared with the mean t28-t56 area reduction (57.64%) observed herein, after 4 weeks of treatment. These data suggest that the choice to increase the treatment time from 60 sec to 120 sec, maintaining a frequency of once a week, led to an improvement in the clinical result. Based on the results obtained, Blue Light appears to reactivate the healing process in acute and chronic wounds that do not respond to standard treatment within 4 weeks. Furthermore, the results for wounds of different etiology, suggests differentiating the treatment scheme, with shorter times for acute wounds and venous wounds. Moreover, it should be emphasized that Blue Light treatment is easy to perform and safe, with no adverse events or side effects.
