Skin ulcers in patients with systemic sclerosis: pilot study.
Authors: Spinella A, de Pinto M, Galluzzo C, Testoni S, Macripò P, Lumetti F, Parenti L, Magnani L, Sandri G, Bajocchi G, Starnoni M, De Santis G, Salvarani C, Giuggioli D.
Title: Photobiomodulation Therapy: A New Light in the Treatment of Systemic Sclerosis Skin Ulcers.
Year: 2022
Publication: Rheumatol Ther 9, 891–905 (2022) https://doi.org/10.1007/s40744-022-00438-9
SUMMARY
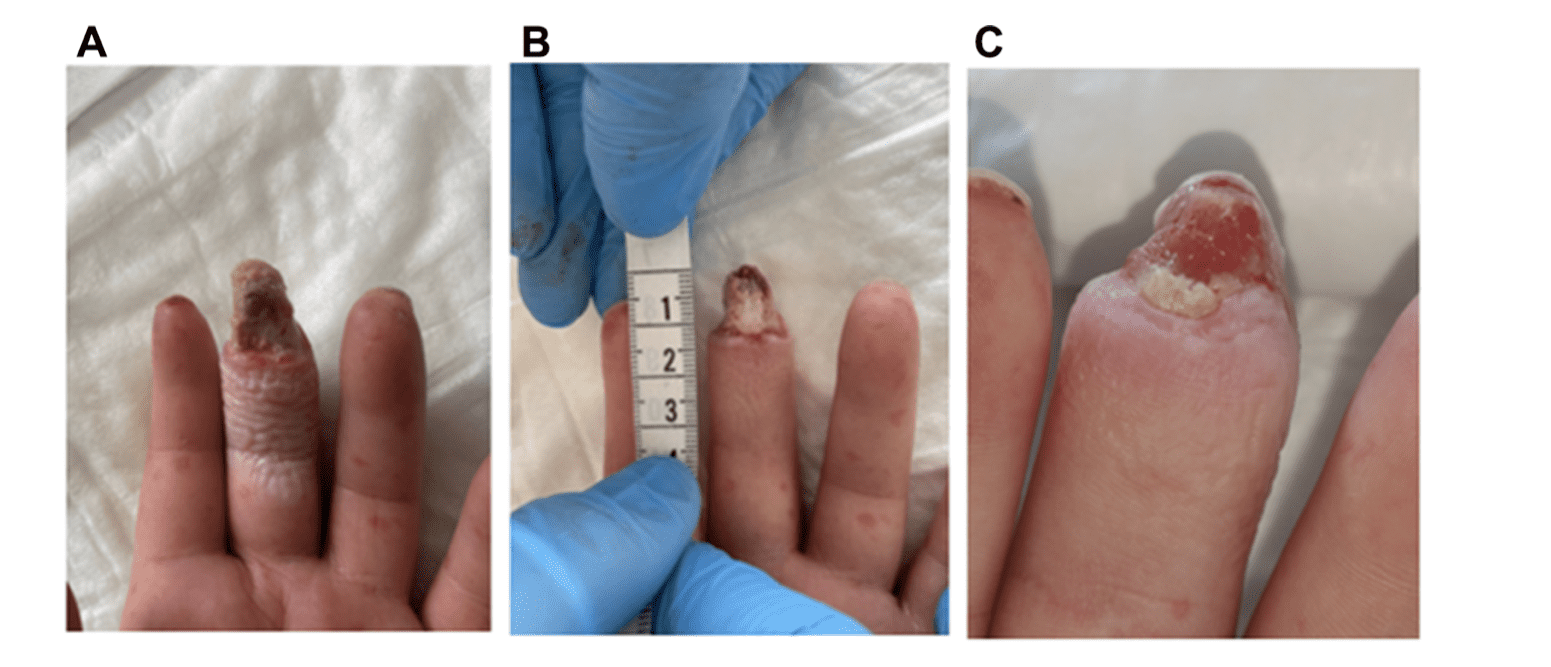
Skin Ulcers (SU) represent one of the most frequent manifestations of systemic sclerosis (SSc), occurring in almost 50% of scleroderma patients. They are frequently responsible for pain and disability, which can severely affect SSc patients’ quality of life. Despite the application of systemic and local treatments, SU sometimes continue to be hard-to-heal lesions. Searching for innovative therapies that support and promote SSc-SU healing is fundamental. In a pilot study, carried out at the Scleroderma Unit of AOU Policlinico di Modena, Italy, a preliminary evaluation of the effectiveness of Blue Light Photobiomodulation therapy (EmoLED) in the treatment of scleroderma skin ulcers (SSc-SU) was performed.
12 SSc patients with a total of 15 digital ulcers, typically located on the fingertips or close to the nails, have been analyzed. Eight SSc patients with comparable SU were also evaluated as controls. All patients were treated with standard systemic therapy for scleroderma vasculopathy, using one or more vasoactive drugs. Local treatment of the SU was carried out according to the wound bed preparation model, mainly based on the TIME framework. EmoLED treatment was performed for 60 seconds every week for 2 months, after wound bed preparation, debridement of the lesion included. SU data (length, width, area, wound bed, perilesional skin features, presence/absence of lesion exudate) were collected after 4 (T4) and 8 (T8) weeks. Each patient was also instructed to record the following data: pain level on a 0–10 mm numeric rating scale (NRS), use of analgesics, possible adverse reactions to the treatment.
Complete healing of SU was recorded in 5/12 (41.6%) of the patients treated with EmoLED during the treatment period. In detail, reduction in SU area (p = 0.012), wound bed improvement (p = 0.019), and reduction of pain (p = 0.054) were observed from T0 to T8 in patients treated with EmoLED. Control patients treated with standard systemic/local therapies merely showed a trend toward an improvement in SU area (p = 0.088) at the end of the treatment period. Furthermore, upon comparing the EmoLED and control group patients from T0 to T8, the authors observed significant differences in SU exudate presence (3/12 vs. 6/8, p = 0.040) and perilesional skin assessment, in particular maceration/erythema presence (1/12 vs 5/8, p = 0.018). Finally, EmoLED treatment was well tolerated by all subjects, none of whom complained about any procedural or post-procedural adverse events from light irradiation.
Based on the positive clinical results and the absence of side effects, the Authors suggest that EmoLED could be a promising tool in the management of SSc-SU, with an interesting role to play in the healing process in addition to conventional systemic and local treatments.